Sugar pills were put in your birth control pack to make the Pope happy
Women have been taking the birth control pill in a way that isn’t the best for nearly 60 years. Strangely, the reason isn’t based on science. Instead, some of the ideas come from the Catholic Church.
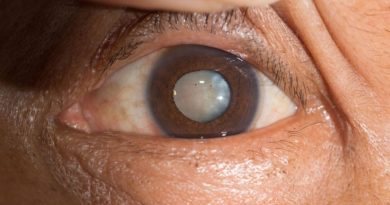
Most oral birth control packets come with seven pills that do nothing. There is no medical reason for this. Every time a woman pops a sugar pill, it reminds her of an unsuccessful attempt to make the Pope happy.
When the first birth control pill came out in the 1960s, it changed the world in a big way. But, like all great medical advances, it wasn’t just medicine that led to its creation.
John Rock, one of the gynecologists who worked on the pill, was a Catholic. He knew that in order for the Catholic Church and its followers to accept the Pill, it would have to be sold as a “natural” way to prevent pregnancy that uses hormones that are already in a woman’s body.
Condoms and other methods of birth control that aren’t natural were frowned upon by the Church, but the rhythm method, in which couples time their sexual activity with certain parts of the woman’s menstrual cycle, was seen as normal and fine.
Jonathan Eig, an American journalist, said that the side effects of hormonal birth control made women think they were pregnant. Rock and his colleagues told women to skip their pills for five days before starting the next pack. This would cause a false period and reassure them that they were not pregnant.
Also, this way of using the pill would make it seem more “natural,” and Rock thought that this might also make the Catholic Church happy. Of course, it was hard to keep track of the days and remember when to start the next pack of pills, so soon there were brands on the market that used sugar pills to mark the off days.
All of those efforts, though, were for nothing when it came to religious acceptance. Years after the FDA gave its OK, in 1968, Pope Paul VI said that all kinds of “artificial” birth control were against church doctrine.
He even tried to say it was a favor to women by saying, “A man who gets used to using birth control may forget the respect he should have for a woman and, ignoring her physical and emotional balance, reduce her to a mere tool for him to use to get what he wants.”
But even though Rock’s attempt to make peace didn’t work, it was already too late. After eight years on the market, “off days” were a standard part of hormonal birth control. These “off days” were often marked with sugar pills, and the withdrawal bleeding they caused was often thought of as a real period, even though they aren’t.
Even though there hasn’t been a long-term study on the continuous use of oral contraceptives, most gynecologists agree that bleeding every month isn’t necessary and that skipping a period is safe.
In fact, there doesn’t seem to be any harm from using them all the time, and new research suggests that skipping a menstrual cycle may be good for women in more ways than one.
A study from 2014 found that headaches, genital irritation, tiredness, bloating, and menstrual pain were better for women who took the pill every day.
Also, some research has shown that long-term use of oral contraceptives can help people with endometriosis better deal with their condition by reducing pelvic pain, increasing sexual activity, and improving the overall quality of life for people with this debilitating disease.
Even though it’s taken a long time, medical guidelines are finally catching up to what we know to be true. The National Health Service (NHS) in the UK is the latest government organization to dispel this common myth.
The institute’s Faculty of Sexual and Reproductive Healthcare (FSRH) has now agreed that there is no health benefit to taking a break from the birth control pill for seven days. This means that this method of birth control can be used every day of the month.
The new guidelines say that consistent use of oral contraceptives “is associated with a reduced risk of endometrial, ovarian, and colorectal cancer,” not to mention the benefits of “predictable bleeding patterns, reduction in menstrual bleeding and pain, and management of symptoms of polycystic ovary syndrome (PCOS), endometriosis, and premenstrual syndrome.”
There is even a theory that long-term use of the Pill can lower the risk of unintended pregnancies caused by “escape ovulation,” but there isn’t enough evidence to back this up yet.
Diana Mansour, vice president for clinical quality at FSRH, told The Independent that the guideline suggests that women could lower their risk of getting pregnant with combined hormonal contraception by taking fewer hormone-free intervals or shortening them to four days.
Not every woman will want to skip her sugar pills, though. Some women might still find it comforting to have their period every month, because it’s a sign that they won’t be having a baby soon.
But we need to give women the right information. Even now, a lot of women don’t know that they can skip their period, and a lot of them still think that if they do, they might be putting their health at risk.
Women around the world should be able to decide for themselves how they want to live their lives. Governments should follow the UK’s lead in this area. It’s the least we can do after decades of wrong information and misunderstandings.